Nursing Homes and Sepsis: How to Protect Residents
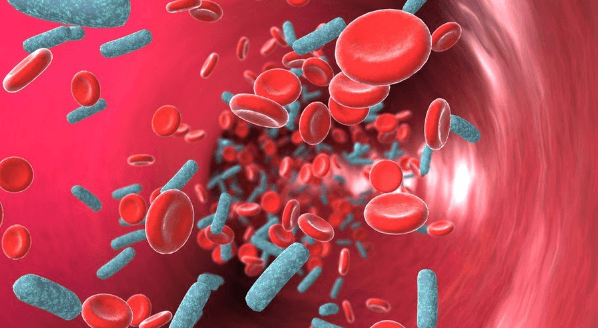
Sepsis is a life-threatening condition caused by a body’s overreaction to infection. Also known as ‘blood poisoning,’ sepsis can be fatal if not treated immediately. Sepsis can lead to tissue damage, organ failure, and death. Septic shock occurs when sepsis is not treated promptly and the patient’s blood pressure drops drastically. Sepsis is a medical emergency on par with strokes and heart attacks.
Any bacterial, fungal, parasitic, or viral infection can lead to sepsis, though the most frequent germs that lead to sepsis are E. coli, staphylococcus, and streptococcus. Sepsis in nursing homes is often a result of bed sores or pressure ulcers.
Who Is Most at Risk of Sepsis?
While no one is immune to sepsis, some populations are more vulnerable to its development than others— and many of these populations can be found in nursing homes. These vulnerable populations include people who—
- Are ages 65 and up
- Are prone to bed sores
- Are severely injured (e.g., burns or open wounds)
- Have a comorbidity like diabetes, kidney disease, or cancer
- Have breathing tubes and catheters to manage blood flow
- Have a weakened immune system
- Reside in the ICU
Nursing home residents often meet more than one criterion for a higher risk of septic shock. Therefore, it is up to on-site nurses and care staff to monitor all residents and report changes or issues immediately.
Signs and Symptoms of Sepsis
Staff members should be trained extensively on recognizing sepsis and septic shock warning signs. On-site nurses must ensure everyone is familiar with the symptoms and understand the dangers so that the response is immediate if sepsis does occur.
The first thing to watch for is the presence of bed sores or other illnesses and injuries. With proper care, these are more likely to not develop into sepsis. However, especially in vulnerable populations, sepsis can occur despite the nursing staff’s best efforts in care.
Warning signs that sepsis is beginning to set in are clammy skin; confusion or disorientation; extreme pain or discomfort; fever, shivering, or extremely low body temperature; high heart rate or weak pulse; and shortness of breath or rapid breathing. Nursing home staff can also watch for “sepsis rash,” a condition where tiny red spots appear on the skin. These ‘red spots’ are blood vessels bursting and clots forming because sepsis has interrupted the blood flow to major organs.
Signs that the patient is going into septic shock include requiring medication to maintain systolic blood pressure and elevated lactic acid levels in blood samples.
Surviving Sepsis
Time is of the essence if a patient develops sepsis. Nursing home staff must provide medical attention immediately and contact emergency services. A resident can die in as little as 12 hours if left untreated. The elderly in nursing homes have weaker immune systems, to the point that a World Journal of Critical Care Medicine study found the fatality rate up to 60% in the target demographic. The National Library of Medicine adds that nursing home residents with severe sepsis will have significantly longer hospital stays, significantly higher rates of ICU admission, and higher rates of death.
However, the numbers are not as grim for mild sepsis. If the condition is caught and treated, fatality rates drop to 40%.
Sepsis can be treated through medication, supportive care, and potential surgery. Medicating for sepsis requires a mix of antibiotics, IV fluids, and vasopressors. IVs need to be started immediately to help hydrate the patient and improve blood flow. Broad-range antibiotics follow to target infections. Doctors will later use blood test results to tailor the antibiotics better. Vasopressors can help raise blood pressure if it remains low. In some cases, insulin is used to maintain blood sugar, or painkillers are administered for the patient’s comfort. Doctors in charge of care will tailor additional medications as needed.
Patients who survive sepsis are at significant risk of developing it again. Therefore, once treatment has concluded, the patient should be monitored even more closely for infections that could lead to a re-infection.
How Nursing Home Neglect Can Lead to Sepsis
Sepsis can develop rapidly, but most infections are gradual. Medical staff should be able to recognize the signs and treat infections before sepsis occurs. While a case of sepsis is not an immediate case of nursing home neglect, it can be a significant red flag that requires investigation to be certain.
Nursing home abuse occurs at an alarming rate in facilities across the US. This abuse can be malicious, but it can also be a matter of neglect. Neglect leading to sepsis can be a combination of issues, from poor training in proper protocols to infrequent repositioning of bed-bound patients or wheelchair users.
Training and communication errors can lead to spreading infections, misuse of personal protective equipment, poor wound care, and improper hygiene and sanitation care for residents. Infections can be highly contagious, so not following best practices may result in a full outbreak. If a healthcare professional misdiagnoses a patient, then that patient won’t receive the proper care. Nurses and care staff must ensure that they are correctly advocating for their patients so that doctors understand the severity of symptoms.
What to Do if You Suspect Abuse or Neglect
Nursing home care staff are a patient’s first line of defense and aid. They are responsible for handling daily needs and medical issues, but they also need to advocate for vulnerable residents who cannot advocate for themselves. Advocation isn’t limited to speaking with doctors or nursing home management— care staff also need to advocate for their residents by reporting any concerns about other staff. The sooner neglect or abuse is noticed, the sooner the offending worker can be released, and the residents can receive proper care through all shifts.
Family members are the next source of help. If you suspect your loved one is being abused or neglected, you need to seek help. Adult Protective Services is the first stop after an incident like hospitalization from sepsis. They will conduct an in-depth review to gather evidence and determine if the case was or was not criminal abuse. If it was, they will handle the rest. If it wasn’t, you will want to reach out to a nursing home abuse organization for a case evaluation. These organizations can partner you with a local attorney to pursue a civil case.
What matters most is ensuring that your patient or loved one is receiving the best possible care.




